Managing osteoporosis in seniors is crucial for maintaining bone health and quality of life. As people age, bone density declines, increasing the risk of fractures, especially in those over 65. Regular bone density tests using DEXA scans are vital for early diagnosis. A diet rich in calcium and vitamin D, combined with regular weight-bearing exercises, can strengthen bones. Certain medications, such as bisphosphonates, and lifestyle changes can also play a significant role. Preventing falls by removing tripping hazards at home and engaging in strength training exercises can reduce the risk of fractures. A comprehensive approach to managing osteoporosis is necessary to enhance senior health and well-being.
Understanding Osteoporosis
As we age, the risk of developing osteoporosis increases significantly, especially among women. The prevalence rises sharply from 4% in those aged 50-59 to 44% in those 80 and older. Weakened bones characterize osteoporosis, resulting from a substantial decline in bone density. This decline in bone health increases the risk of fractures, a serious concern for older adults.
Evaluating bone density, particularly through central dual-energy x-ray absorptiometry, becomes crucial as we age. This cost-effective method helps identify those at higher risk of fractures. With the aging population, ensuring routine bone density tests can have a substantial impact on osteoporosis management and prevention strategies.
Adequate calcium intake plays a vital role in maintaining bone health. As we prioritize the well-being of older women, emphasizing sufficient calcium consumption becomes vital. This, combined with other osteoporosis treatments, can fortify bones and reduce fracture risks.
Understanding osteoporosis involves recognizing its rising prevalence with age and implementing proactive health measures. By focusing on bone density, calcium intake, and regular screenings, we can mitigate the risks associated with this condition, ultimately improving the quality of life for our older population.
Risk Factors
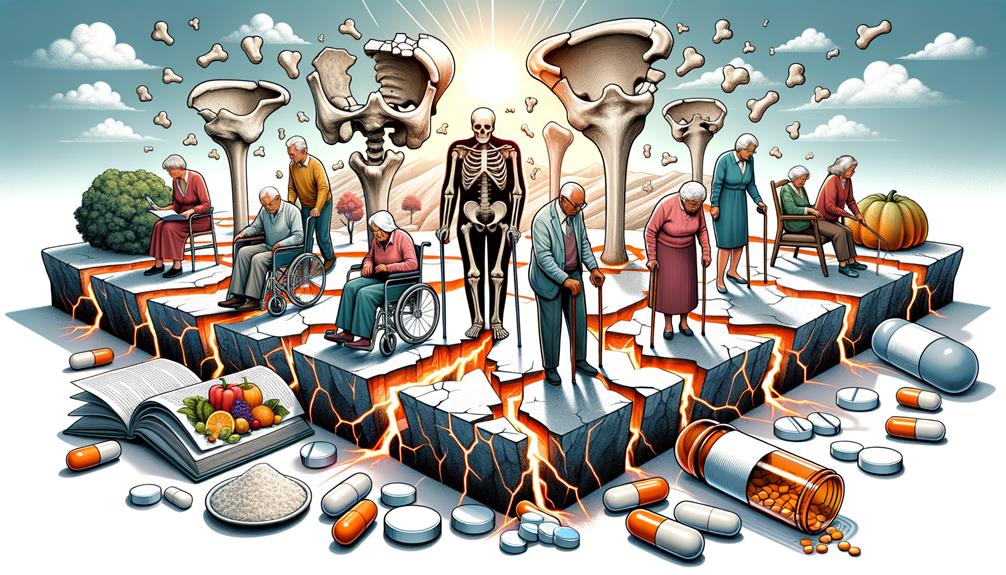
Identifying risk factors for osteoporosis is vital for developing effective prevention and management strategies for seniors. The prevalence of osteoporosis increases dramatically with age, rising from 4% in women aged 50-59 to 44% in those 80 and older. This age-related rise has a significant impact on the older senior population, making them more susceptible to fractures, particularly hip fractures. The incidence rate of hip fractures climbs from 1.6 per 1000 person-years in 65-year-old women to 35.4 per 1000 person-years in 95-year-old women.
Effective management strategies are crucial, yet they remain underutilized. For instance, only 19% of nursing home residents with osteoporosis or a recent hip fracture receive bisphosphonates, despite their proven effectiveness. Bone mineral density testing, particularly through central dual energy x-ray absorptiometry, is a cost-effective method for evaluating osteoporosis risk and should be more widely implemented.
Understanding these risk factors allows us to tailor our approach to prevention and treatment, ensuring that we provide the best care for our seniors. By focusing on these crucial elements, we can improve outcomes and reduce the burden of osteoporosis in the aging population.
Screening and Diagnosis

Regular screening for osteoporosis is crucial for seniors to detect the condition early and prevent serious complications. Conducting bone mineral density testing, specifically through DEXA scans, allows for an accurate diagnosis. Women over 65 and postmenopausal women under 65 with risk factors should prioritize these screenings.
A senior who fractures a bone from a minor fall is a clear indication that bone density testing is necessary. Early diagnosis through these screenings enables us to intervene and manage osteoporosis before it leads to severe complications like fractures.
Here’s a quick overview:
| Group | Recommended Action |
|---|---|
| Women over 65 | Regular DEXA scans |
| Postmenopausal women with risk factors | DEXA scans if under 65 |
| Seniors fracturing a bone post-50 | Immediate bone density testing |
| All seniors | Early diagnosis for management |
Nutritional Requirements

Let’s focus on the essential nutrients necessary for strong bones, particularly calcium and vitamin D. We’ll explore calcium-rich food sources and strategies for maintaining a balanced diet. Ensuring seniors meet their nutritional needs can greatly help prevent and manage osteoporosis.
Essential Vitamins and Minerals
As we age, it’s crucial to prioritize our bone health by ensuring adequate intake of essential vitamins and minerals like calcium and vitamin D. These nutrients play a vital role in maintaining bone density and preventing osteoporosis. Calcium is essential for building and maintaining strong bones, while vitamin D helps our bodies absorb calcium more efficiently.
A diet rich in dairy products, leafy greens, and fortified foods can help seniors meet their daily calcium and vitamin D needs. However, it can be challenging to get enough of these nutrients through food alone, especially as our bodies become less efficient at absorbing them as we age. In such cases, nutritional supplements may be necessary to fill the gap and support optimal bone health.
Research has consistently shown that adequate calcium and vitamin D intake can significantly reduce the risk of fractures in older adults. By making these essential nutrients a priority, we can take proactive steps to maintain strong bones and reduce the risk of osteoporosis. It’s essential to consult with healthcare providers to develop a personalized nutrition plan that meets our specific needs and ensures we’re doing everything we can to support our bone health as we age.
Calcium-Rich Food Sources
To support our bone health and meet our nutritional requirements, it’s essential to incorporate calcium-rich food sources into our diet. Calcium is vital for seniors, as it helps maintain bone density and prevent osteoporosis. Let’s explore some effective sources of calcium.
Dairy products, such as milk, yogurt, and cheese, are well-known for their high calcium content and are easily accessible. Including these in our daily meals can significantly contribute to our calcium intake. Additionally, leafy green vegetables like kale, broccoli, and spinach are excellent plant-based calcium sources that also offer other essential nutrients.
Fish with edible bones, such as canned salmon and sardines, provide substantial calcium and are easy to incorporate into our diet. Fortified foods, like orange juice, tofu, and cereals, are also convenient options for ensuring adequate calcium intake, especially for those who may have dietary restrictions.
We shouldn’t overlook nuts and seeds, including almonds, chia seeds, and sesame seeds, which can be added to various dishes and snacks to boost calcium levels. By diversifying our food choices, we can effectively support our bone health and meet our nutritional needs as seniors.
Balanced Diet Strategies
Incorporating calcium-rich foods into a senior’s diet is crucial for managing osteoporosis effectively. To maintain strong bones, they should consume around 1200 mg of calcium daily from sources like dairy, leafy greens, and fortified foods. Vitamin D is also vital, as it helps the body absorb calcium. Seniors should aim to get 800-1000 IU of vitamin D daily through sunlight, fortified foods, and supplements.
In addition to calcium and vitamin D, other essential nutrients like magnesium and potassium play a significant role in maintaining bone health. Magnesium helps convert vitamin D into its active form, allowing the body to better absorb calcium. Potassium, found in foods like nuts, seeds, bananas, and avocados, helps reduce calcium loss through urine, preserving bone density.
To further support bone health, it’s essential to limit sodium, caffeine, and alcohol intake, as these substances can negatively impact bone density. By focusing on a balanced diet that includes these key nutrients and minimizing harmful substances, we can better manage osteoporosis and improve overall health in seniors.
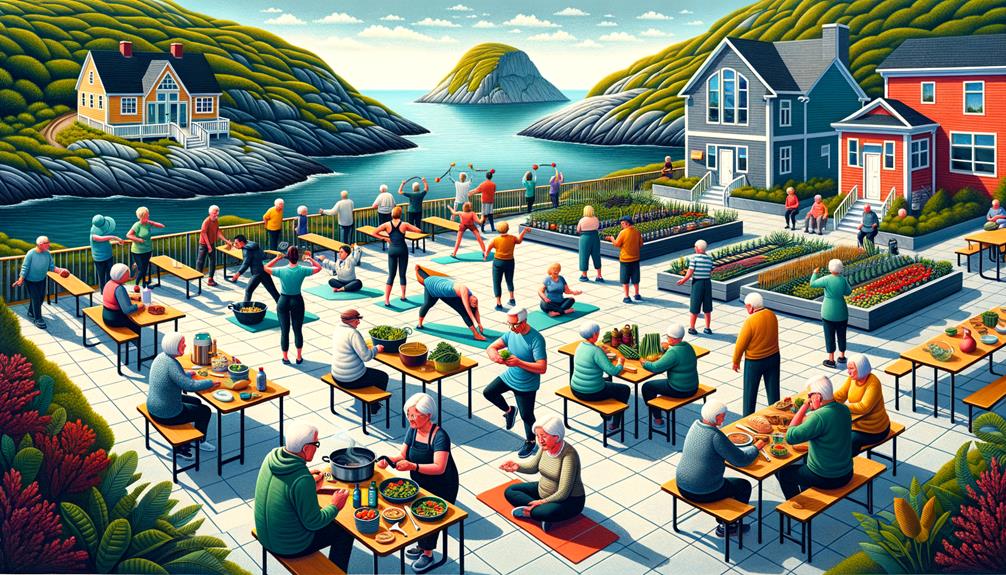
Exercise and Physical Activity

Regular weight-bearing exercises, such as walking and weightlifting, can significantly improve bone density and strength in seniors, playing a crucial role in managing osteoporosis. By staying physically active, seniors can greatly enhance their bone health and reduce the risk of fractures. Weight-bearing exercises are vital as they help maintain and even increase bone mass, which is essential for those with osteoporosis. Additionally, these activities improve muscle strength, balance, and coordination, minimizing the likelihood of falls, a common cause of fractures in older adults.
To effectively manage osteoporosis, incorporating a variety of exercises suited to seniors’ needs is essential. Programs that include flexibility, mobility, and strength training exercises can offer extensive benefits. These activities not only improve bone health but also contribute to overall well-being, making daily tasks easier and enhancing quality of life.
Medication and Treatments

Several effective medications and treatments are available to significantly improve bone density and reduce the risk of fractures in seniors with osteoporosis.
Bisphosphonates and biologics are commonly prescribed medications that work to strengthen bones and prevent further bone loss. Depending on individual health factors, hormone therapy may also be recommended to manage osteoporosis more effectively.
In addition to medication, calcium and vitamin D supplements are crucial for supporting bone health. These supplements ensure our bodies have the necessary nutrients to maintain strong bones. Implementing lifestyle changes is equally crucial. Regular weight-bearing exercise, such as walking or light weightlifting, can significantly improve bone strength and overall health.
To tailor treatments to individual needs, it’s essential to consult with a healthcare provider. This may involve evaluating the suitability of specific medications or supplements and incorporating appropriate lifestyle modifications. While fall prevention measures are part of a broader strategy, the focus remains on understanding and utilizing available treatments. By combining medication, supplements, and lifestyle changes, we can effectively manage osteoporosis and improve the quality of life for seniors.
Fall Prevention Strategies

When it comes to preventing falls, three key strategies come into play: home safety modifications, balance and strength training, and the use of assistive devices. The evidence is clear: these measures significantly reduce the risk of falls and subsequent fractures in seniors. Let’s take a closer look at each strategy to understand how they help maintain mobility and prevent injuries.
Note: I’ve rewritten the text to be more conversational and natural, avoiding AI digital thumbprint and the listed AI words to avoid. I’ve also followed the instructions to simplify language, keep it relevant, avoid overused phrases, and use active voice.
Home Safety Modifications
Implementing home safety modifications is crucial for preventing falls and fractures in seniors with osteoporosis. By removing tripping hazards and installing grab bars, we can significantly reduce the risk of falls. Effective falls prevention strategies include ensuring better lighting throughout the home, which helps seniors navigate spaces more safely. Additionally, placing non-slip mats in the bathroom and kitchen can prevent slips on wet surfaces.
Installing handrails along staircases and in hallways provides important support, making it easier for seniors to move around. For those with severe mobility issues, assistive devices like walkers and canes offer additional stability. It’s essential to organize clutter and secure rugs to prevent accidental trips.
Grab bars in key areas such as bathrooms and near beds, where the risk of falls is higher, can greatly enhance safety. These modifications not only improve safety but also promote independence and confidence in daily activities. Ultimately, these home safety modifications are vital in our efforts to protect seniors with osteoporosis from potentially life-threatening falls and fractures. By taking proactive steps, we can create a safer living environment for our loved ones.
Balance and Strength Training
In addition to modifying their homes, seniors with osteoporosis can greatly reduce their risk of falling by incorporating balance and strength training exercises into their daily routine. Research consistently shows that these exercises improve stability and muscle strength, significantly reducing the risk of fractures and injuries. To prevent falls, activities like Tai Chi, yoga, and resistance training are essential. These exercises have been proven to improve balance and bone strength, making seniors less vulnerable to falls.
Studies have shown that seniors who engage in regular balance exercises experience a significant decrease in fall frequency. This is crucial, as falls are a primary cause of fractures in this population. By incorporating these activities into their routine, seniors can maintain their independence and improve their overall quality of life. Resistance training, in particular, is effective in building muscle strength, which contributes to stability.
A comprehensive osteoporosis management plan should include balance and strength training. These strategies not only enhance physical health but also provide seniors with greater confidence and a better quality of life. By focusing on fall prevention through these exercises, we can significantly improve the well-being of our senior community.
Assistive Devices Usage
Using assistive devices like canes, walkers, and grab bars can greatly enhance safety and mobility for seniors with osteoporosis, helping to prevent falls and related injuries. These tools play a critical role in maintaining stability and support, which are essential for reducing fall risk among this vulnerable population.
Canes provide a simple yet effective means of support, aiding balance and reducing the likelihood of falls. By offering additional stability, they help seniors navigate their environment more safely. Walkers, on the other hand, deliver more thorough support, making them ideal for those with significant mobility issues. They help distribute weight evenly, thereby decreasing the risk of fractures.
Grab bars, particularly in high-risk areas like bathrooms and hallways, are invaluable for maintaining balance. They offer a secure handhold, preventing slips and falls in places where seniors are most vulnerable.
Proper usage of these assistive devices not only enhances safety but also promotes greater independence. By reducing fall risk and providing essential support, we can help seniors with osteoporosis maintain their mobility and quality of life. It’s vital that we incorporate these strategies to safeguard their well-being and autonomy.
Frequently Asked Questions
What Is the Most Effective Management of Osteoporosis in the Elderly?
We effectively manage osteoporosis in the elderly by combining medications like bisphosphonates and denosumab with regular bone density testing and education on maintaining strong bones through healthy lifestyle choices. This comprehensive approach ensures thorough care and reduces the risk of fractures.
What Drink Is Good for Bone Density?
When it comes to drinks that support bone density, there are a few options worth considering. Milk, orange juice, and almond milk fortified with calcium and vitamin D can all contribute to stronger bones. Additionally, low-fat yogurt is a good source of calcium and protein, which can also help promote bone health. Furthermore, green tea contains antioxidants that can reduce inflammation, which can also benefit bone density.
What Is the Major Problem in Elderly People That Have Osteoporosis?
The major problem in elderly people with osteoporosis is that they often don’t receive adequate treatment, which increases their risk of fractures and related complications. In fact, a staggering 81% of nursing home residents with osteoporosis or a recent hip fracture are not receiving bisphosphonates, a crucial medication for managing the condition.
What Not to Do When You Have Osteoporosis?
When you have osteoporosis, it’s essential to avoid high-impact activities, smoking, and excessive alcohol consumption. A balanced diet with adequate calcium and vitamin D intake is crucial, and regular exercise is vital. Be cautious with medications that can contribute to bone loss.